- Author : Dr. Shreyanka. M.D, MBBS, DLO, MS, Assitant Professor, Department of ENT, BGS Medical College & Hospital
Migraine is one of the most common causes of repeated headaches accounting for 15-20% of the primary headaches in India. Most of the time it is not diagnosed and not treated correctly.
What is a Migraine?
Migraine is not just a headache, it is a complex neurovascular condition that can cause moderate to severe throbbing/pulsating headaches, often on one side of the head but can be bilateral also. Migraines can last for hours to days and can significantly impact daily routine.
Recurrent migraine episodes usually have a family history and it is more commonly seen in women than men. It starts during early adult life and decreases after the age of 45 years.
Why and how does migraine occur?
The exact cause and mechanism of migraine are not known. It could be due to the overactive nerve cells sending signals to blood vessels resulting in vasodilatation and the release of inflammatory substances stimulating nerves in the brain and spinal cord which sensitises surrounding tissues resulting in prolonged pain.
How to identify migraine?
Headaches are throbbing or pulsating, usually one-sided, but can present on both sides. Migraine headaches will worsen on exposure to bright light, loud noise, strong odours and physical exertion.
Other symptoms include nausea, vomiting, eye pain, blurred vision, dots or halos in the field of vision, increased sensitivity to light and sound, touch and smell, feeling very warm (sweating) or cold (chills), dizziness, ringing sensation in the ears, neck pain, pale look, tiredness, loss of appetite, nose block etc.
What are the triggers for migraine attacks?
-
Stress
-
Anxiety
-
Bright light, flashes of light, sunlight
-
Inadequate intake of water
-
Hunger
-
Lack or disturbed sleep or too much sleeping
-
Over exertion/ tiredness
-
Certain scents/ Strong odours
-
Caffeinated drinks
-
Certain eatables like chocolate, dairy, foods with MSG, foods with tyramine, fruits, meats, onions, nuts, and processed foods.
-
Smoking, tobacco chewing and alcohol intake
-
Changes in the weather such as strong/ cold wind, change in altitude, barometric pressure changes etc
-
Hormonal changes
-
Certain medications causing dilatation of blood vessels
-
Daily or overuse of over-the-counter medications for migraine.
Types of migraine:
a) The most common type of migraine is migraine without aura (Common migraine) seen in 70 – 80 % of the cases.
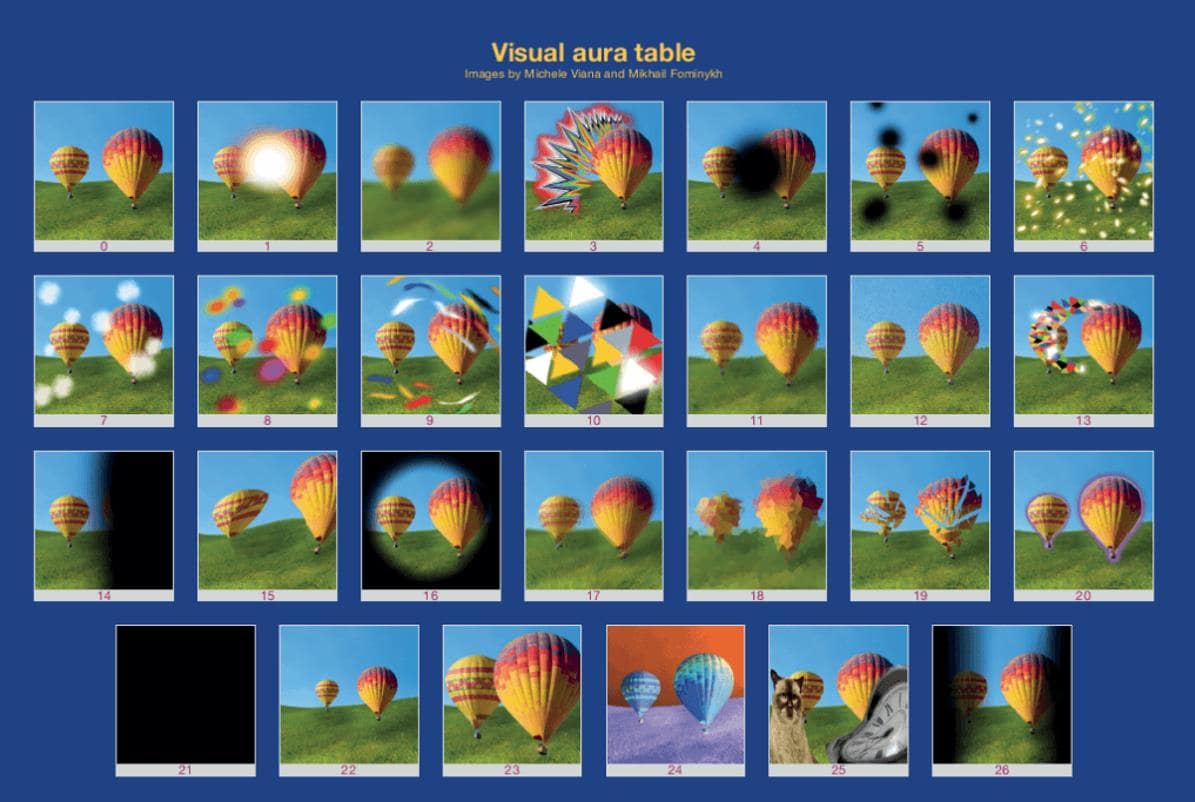
b) Migraine with aura (Classical migraine) – seen in 20 – 30 % of the cases and more severe compared to common migraine. Warning signs occur a few minutes before the attack. The most common aura is visual, which may include positive or negative features. For example: Flashes of light, zig-zag lines, difficulty focusing etc.
c) A silent/acephalgic migraine - presence of other symptoms of migraine without headache.
d) Retinal migraine – usually reversible condition with temporary loss or blurred vision, lasting for minutes to days sometimes even months.
e) Hemiplegic migraine – Presenting with one-sided weakness, loss of sensation etc similar to stroke.
What is a chronic migraine?
The International Headache Society has defined chronic migraines as occurring 15 or more days per month for more than 3 months, with the features of migraines being at least 8 days per month. There will be an increase in the frequency and intensity of the symptoms over some time. Medication overuse is a major risk factor for chronic migraine.
Phases of migraine:
a) Premonitory phase – Can start 24 hours before the actual headache—mood changes, food cravings, brain fog, yawning, disturbed sleep, depression.
b) Phase of aura – Starts a few minutes before the start of the attack. Warning symptoms like visual disturbance, numbness, weakness, confusion, difficulty in speaking, dizziness, and abdomen pain may be present.
c) Acute phase – Actual symptoms phase as described above.
d) Phase of resolution – sudden end of the symptoms. Fatigue, urgent need to sleep etc.
e) Postdromal phase - Following the episode, the patient feels severe exhaustion, fatigue, depression etc, which usually occurs a few hours to 2 days after a headache.
f) Interictal phase – Phase between the migraine attacks without any symptoms.
How do we manage the attacks?
Detailed history is the key to the diagnosis of migraine. However, a complete evaluation is necessary to rule out other causes of headaches which can be life-threatening. Identifying and eliminating the triggering factors helps in managing the episodes. For example:
· Stress and anxiety management like meditation, yoga etc
· Avoid tobacco, alcohol, caffeinated drinks.
· Avoid eatables triggering the attacks.
· Timely and adequate intake of food.
· Adequate intake of fluids.
· Adequate undisturbed sleep.
· Avoid over-the-counter medicines or self-medication
Educating the patients and the attendees about the conditions and the importance of identifying the causative factors can improve their lives significantly. Whenever possible, it is best to consult a specialist. Acute episodes can be treated with medications if taken during the “golden moment” ie early when the headache starts. However, regular use of medicines is not advisable, as it causes worsening and increased frequency of the symptoms over time. Chronic patients will be treated with prophylactic therapies.


